Julie Entwistle, MBA, BHSc (OT), BSc (Health / Gerontology)
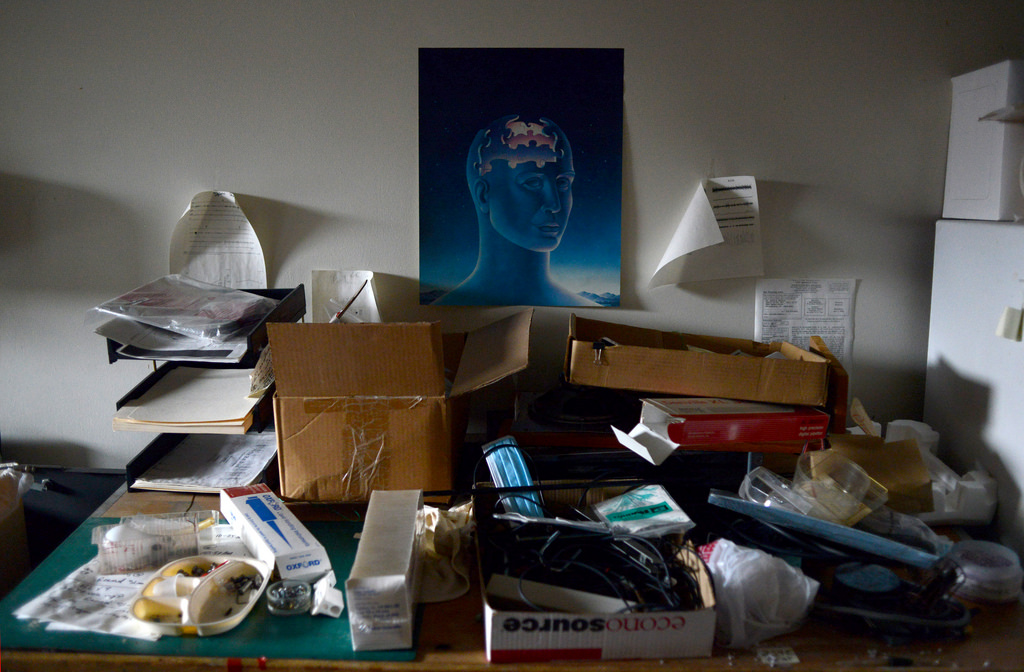
Last stop for Brain Injury Awareness Month – my favorite topic – organization!

Yes, this is my drawer system to store pens, pencils, and markers. And if I find a pencil in the pen drawer look out! Perhaps being organized and knowing how to find what I need when I need it is one of the many ways I manage the demands of being a business owner and mother of four. But the reality is that we all have different levels of energy, tolerance and mental attention and these things can become depleted after a brain injury. So, if you were an energizer bunny with a DD battery before your injury, chances are your new batteries have been replaced with some AAA’s. This means that daily activities will take more time, more energy, and you will need to recharge sooner. So, considering this, do you really want to spend your valuable energy looking for stuff?
Consider that you have 10 units of brain capacity and energy when you wake in the morning. Every activity you have on your “to do” list takes one unit. Going for a walk, preparing supper, managing the laundry, responding to emails, attending an appointment, completing personal care, and having coffee with a friend all drain your battery. Some of these activities are necessary, some can be put off, and others are enjoyable. So what if you spend one unit of energy looking for your phone, keys, that bill that needs to be paid, your agenda, or those new runners you bought yesterday? What activity will come off your list when you have spent your energy to find something that with some organization would have taken you no time at all? Maybe you will call your friend to cancel, or order supper in again. Maybe the laundry will wait to tomorrow, or those emails will just keep accumulating. But this is unnecessary because you had the energy and cognitive ability to manage these things, it just became misdirected.
Often the focus of occupational therapy becomes helping people to organize their activities, their stuff or their time. Schedules and consistency are keys to helping people to understand the size of their battery and the amount of units each activity takes. This can be difficult when working with clients who did not need to be organized before an injury or illness, but the necessity of this following cannot be ignored. Even small steps to help people to be more organized can have a huge impact.
Helping clients with brain injury to become more organized can take many forms, depending on the client, the nature of their problems, and how they previously organized their stuff and their time. What I tend to witness is the time lost and sheer frustration that clients experience looking for cell phones, wallets and keys. Often, cell phones become used as a “second brain” assisting people to maintain a schedule and make appointments (calendar), remember things (task lists), have access to support systems (contacts, calls, text, email), and negotiate their environment (maps and GPS). If this gadget is so important, it is even more important that people know where it is. Having a catch tray by the front door, in their room, or a standard docking station can be helpful. Wallets and keys should also be left in a consistent location. I am sure we can all relate to that feeling of looking for our keys in their usual spot to find they are missing. But if you lack the ability to efficiently look for these, it could completely derail your day.
After the day to day items have a place, then we can work to simplify other spaces that are identified barriers to function. Perhaps the kitchen has become too cluttered to allow for efficient meal preparation, or the bills are piling up because these are lost in a stack of papers. In the world of insurance I find that clients become overwhelmed by paperwork and this results in missed appointments, non-response to time sensitive material, or failure to submit for expense reimbursement. Slowly, over time and with suggestions and tools (filing cabinets, labels, folders, a pen drawer!) clients become able to more efficiently spend their units of energy on things that are more important, or more fun and ideally, learn to transfer these strategies into other life areas independently – like work, school or parenting.
Originally posted June 30 2014
To read more of our articles on brain injury check out our section on Brain Health.